Terrifying.
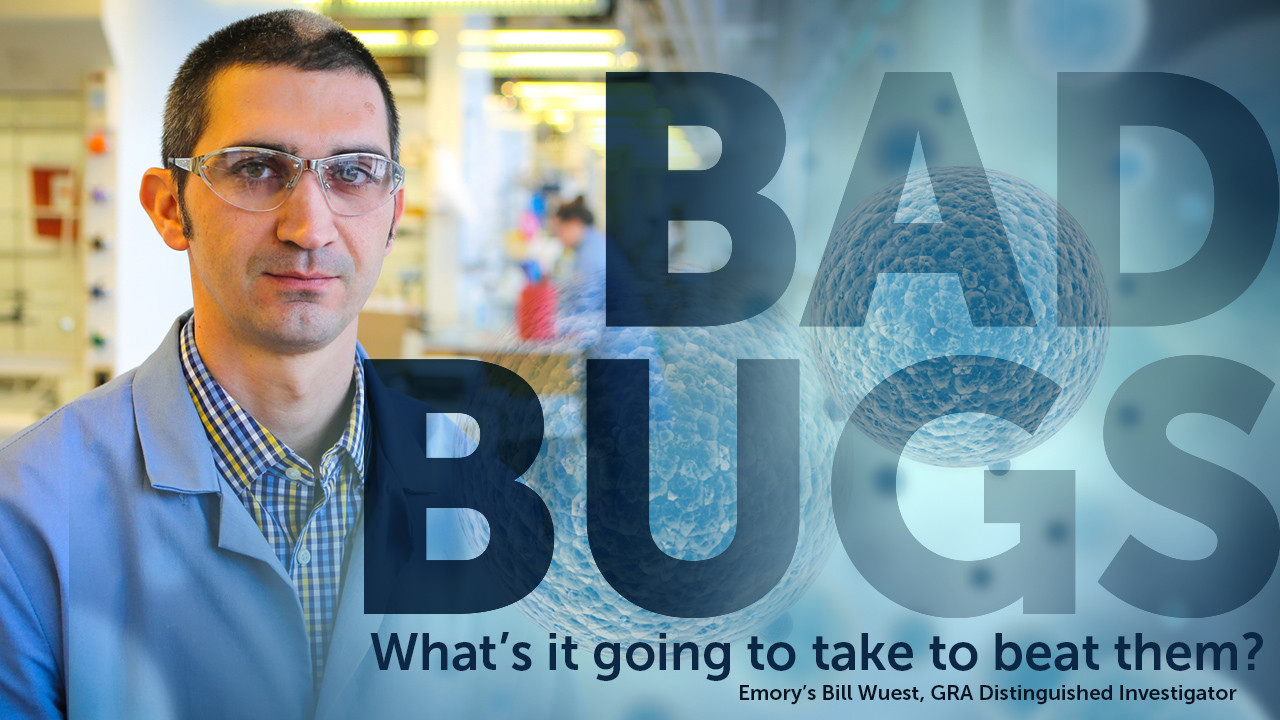
That’s how Bill Wuest describes watching bacteria sidestep an antibiotic.
Using advanced technology, he can actually see how the bacteria are changing their genetic code to stop the drug’s effects.
It’s powerful evidence of how adaptable bacteria are, and a reminder of how tough it is for scientists like him to defeat them.
But Wuest (pronounced “Weest”), who joined Emory University in 2017 as a GRA Distinguished Investigator, is up for the challenge. He’s working on a new arsenal of drugs that can either keep bacteria from going rogue, or disarm them when they do.
He just scored one of his biggest victories yet: he and his collaborators have found a new class of compounds that cure hard-to-clear staph infections in mice, a major finding published in the April 5, 2018 issue of Nature. Someday, these compounds could be used against antibiotic-resistant staph (MRSA) – by themselves or in combination with other drugs.
His research is crucial, and growing more so as bacteria get hardier. Drug-resistant bacteria infect more than 2 million people each year, according to the Centers for Disease Control and Prevention, killing more than 23,000. A 2014 study by KMPG says that by 2050, antibiotic-resistant infections could cause more deaths than cancer. That’s why both the National Institutes of Health (NIH) and the National Science Foundation (NSF) are funding Wuest’s work.
Part of the challenge in drug discovery is simply trying to keep up. Bacteria adapt quickly, but developing a new drug takes a very long time.
Wuest starts by searching through the scientific literature to find compounds – often, chemicals that exist in nature – that have been shown to work against specific bacteria. Then he uses those as inspiration for synthetic compounds likely to have the same effect.
For the new drugs to fight MRSA, Wuest started with compounds called retinoids. His collaborator Eleftherios Mylonakis, of Brown University, had discovered that a few specific kinds of retinoids could kill bacteria in worms infected with MRSA.
Wuest then created “analogs” of these compounds – substances made in the lab that have similar structures to the compounds Mylonakis had tested.
Wuest’s analogs proved to be better than the originals. They were equally good at killing the bacteria, and better at not killing the worms. Testing in mice showed the same encouraging results.
Among Wuest’s other promising research is finding a compound to fight Streptococcus mutans, a bacterial slime that’s mostly known for causing tooth decay, but which can sometimes cause heart disease.
For years, Wuest has been working on a compound based on a natural substance called carolacton. His analog version is much simpler to make than carolacton itself and has proven effective in the lab.

Because he was already working with S. mutans, Wuest’s colleague Marisa Kozlowski of the University of Pennsylvania recently asked him to collaborate on her research of a different compound to fight the same pathogen. A large company had asked Kozlowski to investigate the use of honokiol, a chemical found in magnolia cones, as a possible additive to toothpaste.
Unfortunately, although previous tests had suggested honokiol could stop S. mutans, when Wuest tested it in the lab, it didn’t work.
The surprise: Wuest had chosen other analogs to use as control compounds in the honokiol testing, and one of those was highly potent. Now he’s added it to the analogs he’s researching to defeat the S. mutans slime.
In the world of drug discovery, not all surprises are so welcome. In recent years, Wuest’s lab did extended work on developing a compound that would keep staph bacteria from getting the iron they needed.
The analog Wuest created worked in part by damaging the membranes of the bacterial cells. It was a promising mechanism scientists hadn’t seen before in this class of compounds.
Then came the bad news: The compound also damaged red blood cells. It could never be a viable drug for use in living patients.
That was a big disappointment, Wuest admits, yet he sees it as a natural part of the scientific process.
“That research shows the importance of the work we’re doing,” he said. “It raises a new question for us to investigate. We can develop something that works against the pathogen, but not against the cells we want to maintain.
Obviously, no decent scientist wants to make a drug that does collateral damage to blood cells. But Wuest’s vision of custom-tailored drugs goes further. His ideal drug is one that kills only the specific bacteria it’s designed to fight — not other vital cells, not beneficial bacteria, not even other bacteria that are potentially harmful.
It all comes back to preventing drug resistance. Today, broad-spectrum antibiotics get prescribed for all kinds of infections. While they’re curing the patient, these drugs also kill other bacteria in the body – but only some of them. Those that survive the medicine have a higher likelihood of mutating into superbugs.
A narrowly targeted drug, on the other hand, designed to fight only a single type of bacteria, gets prescribed less often. The less the drug is used, the less other potential pathogens are exposed to it, and the less chances they have to make defensive adaptations. “That should prolong the time to resistance, in theory,” Wuest said.
There will always be a need for broad-spectrum antibiotics, but he would like to see those reserved for the toughest cases, when nothing else has worked.
A pathogen Wuest is targeting now is Pseudomonas aeruginosa, a common cause of lung infections in patients with cystic fibrosis. For several years, Wuest has been developing a drug based on promysalin, a tiny molecule that scientists found in the soil near the roots of rice plants.
Now that Wuest is in Georgia, his promysalin research is getting a boost. Biologist Marvin Whiteley, a GRA Eminent Scholar at Georgia Tech, also studies P. aeruginosa. He and Wuest are excited to work together, both directly and through the research group CF Atlanta.
“Marvin and I e-mail a lot,” said Wuest, his voice giving away his enthusiasm about their connection, which is progressing from like-minded colleagues to full-on collaborators.
The feeling is mutual.
“I collaborated with excellent chemists at UT-Austin,” said Whiteley, “but none were exclusively focused on antibiotic discovery.” With Wuest in Atlanta, Whiteley and the members of his lab have the chance to work with chemists who have the same research goals.
Wuest also looks forward to collaborating with doctors at Emory University Hospital, and with other researchers in Emory’s Antibiotic Resistance Center, a group dedicated to fighting drug-resistant pathogens.
The goal of all his work, whether collaborative or independent, is the same: to create successful compounds that go out of his lab and into the pharmacy.
Part of his motivation is that he wants to translate science into marketable products and viable businesses. Wuest has always had a business mindset – his undergraduate degree from Notre Dame was in chemistry and business – and he takes pride in the successful businesses he’s launched in the past.
But more than that, he wants to help win the superbug battle and save lives.
“I was always intrigued by drug discovery,” he said. “I hate blood, so that ruled out being a doctor, but I always liked the idea of curing people.”