

Got golfer’s elbow? Plantar fasciitis? Some other chronic tendon injury?
Then this procedure from this Emory-Georgia Tech startup may well be in your future.
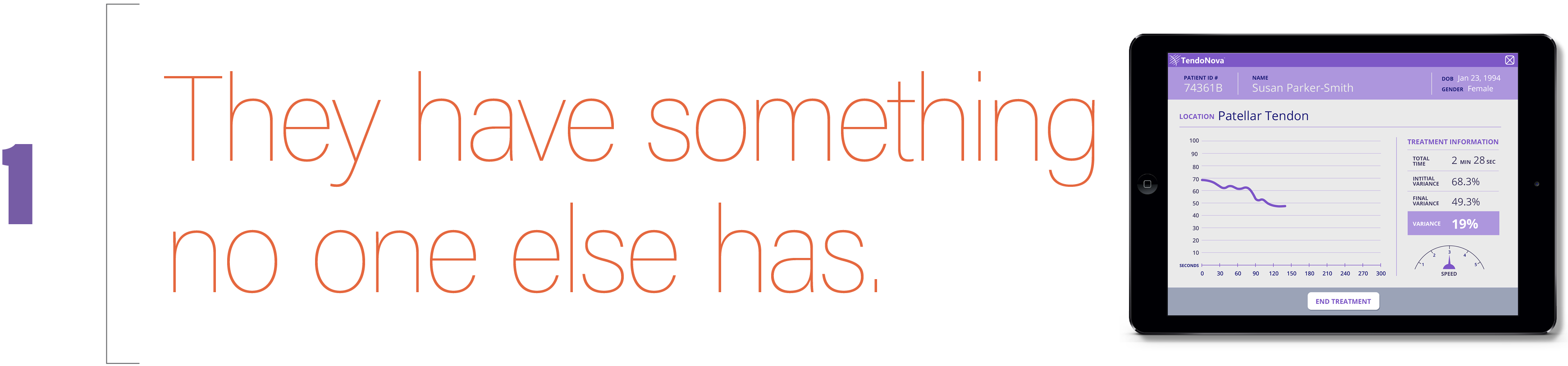
It’s a way for clinicians to see how well they’re doing while they’re treating chronic damage to tendons.
First, some background: A common treatment for chronic tendinopathy is called PNT (percutaneous needle tenotomy). Clinicians take a small gauge needle and poke holes in scar tissue to break it up. Although it’s guided by ultrasound, PNT is only 65% effective, mostly because physicians perform the procedure by “feeling” the effect they have on tissue – and every clinician has a different feel.
By contrast, TendoNova’s Ocelot system uses a sophisticated cutting tool on the scar tissue, which promotes healing. And as the procedure is taking place, clinicians get a real-time view of data, which puts a number to what a clinician “feels.
In June 2020, the NFL Players Association announced it was investing in TendoNova. The added investment will allow the company to complete testing and submit its Ocelot system for FDA approval.
The investment makes sense: Damage to tendons is one of the most common injuries to pro football players. “In fact, chronic tendon injuries can lead to a ruptured tendon, which will most likely end a player’s career,” says Jonathan Shaw, one of TendoNova’s four co-founders.
The NFL also validated TendoNova’s system – the company was one of just five worldwide to present in the NFL’s “1st and Future” competition back in 2019.

In any given year, 30 million Americans suffer from chronic tendinopathy. (That’s a lot of tennis elbow and painful shoulders.) The unmet market need for treatment is estimated to be $1.4 billion.
The most common treatments are conservative – rest and/or physical therapy. But those take many months, and they work for just some patients.
Surgery is effective, but it’s expensive and invasive. PNT and other ultrasound-guided procedures are also prevalent, but there’s that inconsistency problem (see no. 1).
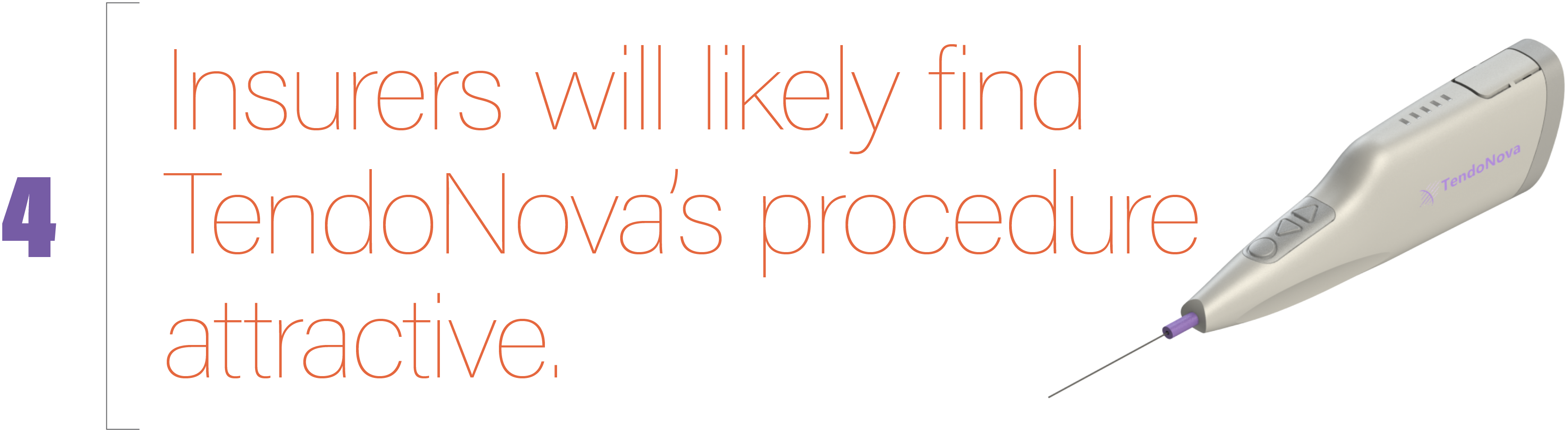
That’s because it fills a key gap in treating chronic tendinopathy.
Here’s how it works: The Ocelot system is a slender handheld device. Its base is a drive unit with built-in wireless technology to transmit data. A disposable sterile shell – with a versatile cutting tool that can be customized, depending on the clinical need – is attached to the drive before each procedure. The cutter is a little like a Dremel power tool.
The beauty of the device is that it provides the precision of surgery, but at a fraction of the cost. “So when a practice files for insurance reimbursement of a procedure using the Ocelot system, insurance providers will find the comparative affordability attractive,” Shaw says.
While training is required, clinicians will no longer have to “feel for when they have treated the tendon enough,” as they do in a PNT procedure. Because the Ocelot system’s data feedback guides precision.
In essence, this is like bringing a surgical procedure to the clinician’s office. The small footprint and reduced cost make in-office procedures economical for the patient and physician.. (Hence, the ease of use and economics serve to expand the market.)
Beyond Ocelot, TendoNova plans a suite of tools and devices for a range of in-office orthopedic procedures.
TENDONOVA CORP.
Website >
Launched: 2017
Ocelot approved by FDA: March 2022 • Details >
GRA investments: Phase 1 and 2 grants totaling $200,000. Jonathan Shaw: “GRA provided our first and second investments. They really enabled us to get off the ground.”
Chairman: Lou Malice, a medical device executive with 30+ years of experience in commercialization, R&D, manufacturing, supply chain, and regulatory.
Intellectual property: Two patents (one issued, one pending)
Other investors: NFL Players Association, angel investors, private individuals.
Origins: A former physical therapist, Jonathan Shaw had the idea while pursuing his master’s degree in biomedical innovation and development at Emory-Georgia Tech’s Wallace H. Coulter Department of Biomedical Engineering.
He enlisted the help of three other students (Shawna Khouri, Brett Rogers, Luka Grujic) to develop the invention as their master’s project. In doing so, they collaborated closely with clinical experts in the field, Dr. Ken Mautner (Emory) and Dr. Gerald Malanga.